OP-ED Where Do We Go from Here?
Medical Director, Recovery Management Services
Vault Workforce Screening, A Sterling Company
Firstly, I want to thank all of you for reading and for all you do as Involved MROs. Our profession along with the whole field of workplace drug testing is going through a significant evolutionary process. Public sentiment about substance misuse seems to be shifting, and regulatory changes are attempting to keep pace. Additionally, we've just had an election, the results of which may have long reaching effects on federal and non federal workplace drug testing. I'm one of the old guys. I've been an MRO since 1992 and I've been involved in various aspects of MRO practice since then including teaching, consulting, testifying and serving as a Director on the MROCC Board. So, as I approach the latter part of my career I'm going to throw out some ideas. These are mine and are not reflective of the MROCC Board, any governmental agencies, or even probably some of my friends and cohorts, but I hope at least they facilitate thought and ongoing discussion.
I should start by letting you know that I am an addiction medicine physician, not an occupational medicine physician like many of you. I came into this profession with what may be a different perspective. Not only am I focused on public safety, but I also saw workplace drug testing as an opportunity for an early intervention that could help to address the process of addictive disease. Robert DuPont authored a paper in 1995 suggesting that with all the donor protections of most workplace testing programs, 93% of those who do test positive in those programs may be suffering from an addictive disorder.1
I still believe that and that's why I'm concerned about the future of the MRO profession and of forensic drug testing as a whole. We've all seen tremendous changes even if you haven't been around as long as I have. Federally regulated drug testing now makes up only about 15% of the total volume of workplace testing. MRO training courses have declined both in numbers and attendees and subsequently numbers of certified MROs have declined as well. So have MRO jobs and income from MRO practices. Financially, workplace drug testing has been a race to the bottom, and we are leading the economic decline. On top of that there is now the very real likelihood that the federal government will join many states and de-schedule marijuana. What will happen to workplace drug testing when the substance causing the vast majority of workplace positive results is either no longer able to be tested for or disregarded if it is? Additionally, public attitudes are finally changing about people who misuse substances. Happily, we no longer live in a world of good guys and bad guys. We are evolving in the belief that substance misuse and addictive disease are worthy of treatment not stigma. This evolution in attitudes will continue to affect workplace testing programs moving forward. I believe we are rapidly approaching a time when the mere presence of a positive drug test result will not be the only deciding factor in an employment decision. The decision point will be whether that donor can do the job or not. This means that to survive as an industry, workplace drug testing and MROs will need to join in becoming a fit for duty decision making platform. We can no longer rely simply on a positive drug test result being per se evidence that the donor is not fit to go to work.
I may separate myself here from many of my cohorts because I relish this evolution and I think it is long overdue. Although MROs have always been required to be physicians, for much of today's MRO practice arguably a medical degree is not required to do the job. Dr. Pohlman has authored several recent pieces in the newsletter about her work with the NRC, and that work gives us an idea about what an expanded MRO role can look like. My daily practice is recovery monitoring primarily for health care professionals, and this is another example of how basic MRO knowledge can be expanded beyond what is taught in most MRO courses. In my practice I am not only concerned for public safety. My practice also supports highly qualified doctors, nurses and other health care professionals as they recover from addictive disorders and as they return to the practices they are trained to perform. This requires more advanced MRO knowledge and arguably should be done by people with medical degrees. That also makes this kind of MRO practice much more interesting.
I believe that workplace drug testing in general and MROs in particular should support the evolution of our profession toward a fit for duty entity that combines the interpretation of laboratory toxicology with other aspects of fit for duty decision making and the team members that perform those functions. I would hope this evolution will involve courses of instruction and certification exams that go beyond the simple basic MRO practice that we have today.
Please feel free to offer counterpoints and discussion if you want to, and I hope you all enjoy the discussion.
FOOTNOTES
MRO Responsibilities Under
10 CFR 26 (NRC) Fitness for Duty Regulation:
Alcohol Misuse and Abuse
Previous issues of the MROCC MRO Quarterly Newsletter included a detailed discussion of the MRO role in determining subversion vs. substitution and adulteration and legal medication misuse under Nuclear Regulatory Commission (NRC) regulations (10 CFR 26). Differences in MRO interpretation of confirmed test results under NRC regulations versus other Federal workplace drug testing programs (DOT, HHS) were discussed. Another major difference between 10 CFR 26 and the other federally regulated workplace drug testing programs is the role of the nuclear MRO/ Substance Abuse Expert (SAE as defined in 10 CFR 26.187) in alcohol testing. Other federal workplace drug testing programs completely exclude the MRO from the interpretation of alcohol testing results.
Regarding the SAE and alcohol testing, NRC regulations state the following:
§ 26.187 Substance abuse expert
NOTE: It is common in the nuclear industry for MROs to also be qualified as SAEs.
§ 26.27 Written policy and procedures
§ 26.31 Drug and alcohol testing
§ 26.99 Determining the need for a confirmatory test for alcohol
In addition to the mandates described in the regulations noted above, the MRO/SAE may also be requested by the nuclear workplace to review the results of any non-zero alcohol test (< 0.01%) and make a determination of fitness even though the level is not a violation of the regulation. Any detectable level of alcohol is a potential "misuse" of an over the counter drug (alcohol) and may be handled as discussed in the MROCC MRO Quarterly 2024 issue #3 newsletter regarding NRC regulations covering medication (and other legal substances) misuse.
Brief overview of alcohol statistics, use definitions and references
- Per the National Center for Substance Abuse: "Though legal, alcohol kills over 95,150 Americans every year...Among the 15 million individuals with Alcohol Use Disorder (AUD), less than 8% receive treatment."
- Over 70,000 drug (all drugs, excluding alcohol) overdose deaths occur in the US annually. https://drugabusestatistics.org/
It may be a surprise to know that alcohol related deaths per year in the US exceed all types of other drug related deaths combined. In the workplace, including those that are federally mandated to perform workplace drug testing, alcohol is by far and away the most common substance of abuse.
Definitions of alcohol use (measured as "standard drink" use) include the following:
Moderate use - men, 2 per day or less; women, 1 per day or less
Binge use - men, 5 or more in 2 hours; women 4 or more in 2 hours
High intensity use - two or more times the binge use amount per gender
Heavy drinking - men, 5 or more on any day, 15 or more in a week; women, 4 or more on any day, 8 or more in a week
https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking/
https://www.niaaa.nih.gov/sites/default/files/publications/NIAAA_Binge_Drinking.pdf
https://www.cdc.gov/alcohol/about-alcohol-use/index.html
When interviewing donors regarding their use of alcohol, it is critically important to verify the amount of alcohol consumed. Most donors do not understand the concept of a "standard drink" (see links below), thus, their perception of alcohol consumed varies significantly from the reality of their consumption. Example: A single "tall boy" beer may contain 16-40 oz and have and have an ABV content of 4-15%! However, there are exceptions. Scotland produces the world's strongest beer: Brewmeister Snake Venom, which has 67.5% ABV.
https://www.cdc.gov/alcohol/standard-drink-sizes/index.html
https://rethinkingdrinking.niaaa.nih.gov/tools/calculators/drink-size-calculator
When interviewing donors regarding BAT levels that are less than 0.02% that are considered negative per NRC regulations (often referred to as "blowing numbers"), but still possibly indicative of alcohol misuse or abuse, it can be helpful to utilize an online BAC calculator (eg, https://celtickane.com/projects/blood-alcohol-content-bac-calculator/). Recommending that the donors do the same can help them understand their BAT result and the amount of time required to achieve a BAC of 0.00%.
Finally, don't forget that alcohol withdrawal and hangovers can cause impairment even when the BAT is 0.00%. Clearly such a situation is misuse and probable abuse of alcohol.
Now some case studies to see how the MRO/SAE may interpret and implement 10 CFR 26 Fitness for Duty regulations regarding alcohol "misuse."
Alcohol Misuse (not confirmed positive) Case Studies
CASE #1
Donor (employee) reported consumption of "two beers" while playing X Box with his son the evening before work. There was no history of prior alcohol use issues, i.e. DUI or other alcohol related arrests. He was in bed by 10:00 pm, work the next morning began at 7:00 am. A random drug screen, including BAT was performed after he arrived for work. Drug screen was negative, BAT showed 0.014%, approximately 10 hours after cessation of drinking (donor weighed 300 pounds). Upon closer questioning, donor revealed that the beer ingested was "Wild Child #5," each bottle containing 750 ml (25.36 oz) with ABV 8.2%.
Donor was informed that his pattern of drinking was consistent with binge drinking. He expressed remorse and appeared unaware that his alcohol consumption was excessive, as he hadn't felt intoxicated. He had developed tolerance to the effects of alcohol. The MRO/SAE recommended that he leave the workplace for the day, return without restrictions the following day and attend an EAP evaluation. Donor was compliant with all recommendations, completed four counseling sessions regarding alcohol use and was placed in follow-up testing. There were no further issues.
CASE #2
A former nuclear industry employee returned to work as a contractor. During the expected pre-access test (pre-employment test per other federal regulations) at 7:40 AM he had a BAT of 0.014%. There was no history of prior alcohol issues, past work history showed no problems. He reported having a "couple of drinks" (at least two) containing whiskey, amount not measured but approximately "two fingers" (at least doubles, likely more). Testing was completed approximately 12 hours after drinking cessation.
Donor was informed that his pattern of drinking was consistent with binge drinking. He was not aware that his alcohol consumption was excessive. As a contractor, donor was not eligible for the company sponsored EAP program. Instead, he was required to complete 12 hours of online substance abuse education prior to reconsideration for access (one such program can be found at https://www.alcoholdrugclass.com/nuclear). He did so, was recommended for access and follow-up testing. There were no further issues.
CASE #3
Donor (contractor) had a random BAT of 0.019% 3 hours after the start of his 7:00 am work shift. NOTE: If the BAT had been performed only 2 hours after the start of his work shift, his BAT would have been > 0.02 and the result would have been a confirmed positive test for alcohol. See 26.103(a)(3) noted above. There was no history of prior alcohol issues but he did have a distant past arrest for possession of marijuana. Per evaluation by an external certified addiction counselor, he reported being out drinking the previous night, consuming 4 shots of vodka and 5-6 twelve once beers between 5:00 pm and 9:30 pm. He had no feeling of intoxication and did not feel under the influence the next day.
Again, binge drinking was noted, with an increase in tolerance. However, he did not meet DMS-V criteria for AUD (alcohol use disorder). He was recommended to complete a drug and alcohol education program. MRO/SAE recommended completion of 12 hours of online substance abuse education prior to reconsideration for access. He did so, was recommended for access and follow-up testing. There were no further issues.
Final Comments
There is no question that alcohol misuse and abuse is the most common substance abuse issue in the U.S. nationwide and in the safety sensitive workplace. Alcohol related deaths kill more Americans annually than all other drug related deaths combined. Currently, the number one reason for liver transplants in the U.S. is alcohol associated liver disease.
It is rare in the nuclear industry to find workers in violation of the 5 hour abstention rule, consume alcohol during their tour of duty or consume alcohol on site. However, it is common to find workers unaware of the definition of a "standard drink" and the definitions of alcohol use: moderate use, binge use, high intensity use and heavy drinking.
10 CFR 26 (NRC) Fitness for Duty regulations for workplace drug and alcohol testing gives employers and MRO/SAEs the opportunity to detect problematic alcohol use early, before a worker develops an alcohol use disorder. All MROs working in the nuclear environment are encouraged to become qualified as SAEs and to utilize a preventive, proactive process in dealing with alcohol issues in the workplace.
Opium's Pathway to Fentanyl
CRL's Fentanyl Results in Urine and Oral Fluids
Introduction
Narcotic abuse has been a problem for centuries all over the world. Opium became a problem in East Asia during the 7th century and Europe in the 1800's. The ability to manage the opium problem back then was ineffective and we see a similar ineffectiveness in the U.S. today.
Opium Background
Opium has been referred to as "poppy tears" since it is derived from the dried latex in the seed capsule of the opium poppy Papaver somniferum. The seeds date back to 5000 BC with records going back to 2100 BC.
Poppy opium extract was already used for pain relief by the 1st century, however opium was not introduced into China for medical use until the 7th century. By the 15th century, the Chinese elites adopted opium as a recreational drug. England began using opium in the 1800s for treatment of cholera and dysentery to replace arsenic and mercury. Even in the U.S., opium tinctures for control of intestinal spasms and diarrhea were available without a prescription until 1970.
Countries near the Mediterranean Sea were the initial locations for poppy crops used for opium trade to China in exchange for spice, tea, and other products. Major trading of opium was advanced by the British East India Company which was chartered by Queen Elizabeth I in 1600 as a private business. At its peak, the British East India Company employed an army of 200,000 soldiers plus war ships to protect and expand their trading to the Far East. In 1874 it was dissolved following nearly 300 years of existence.
Opium Wars
The British East India Company controlled the illicit opium trade to China until the mid-1800s with estimates of up to 30% of the Chinese population addicted to opium. The Qing Dynasty tried to control addiction by banning opium four times between 1829-1831 without success. The issues came to head in 1839 when the Chinese government destroyed 1,400 tons of opium. The East India Company responded with 20,000 troops and harbor blockades to defeat China. The First Opium War ended in 1842 with the Treaty of Nanking which gave Hong Kong island along with $21million as payment for the opium financial losses to the British East India Company. The Second Opium War (1856-1860) occurred over the legalization of opium, opening ports, travel, and trade by Britain and France. Hong Kong was finally returned to China in 1997 after 155 years as conditions of the treaties.
But the British were not the only ones who benefited from the opium trade. The United States sourced their opium largely from Turkey for trade with China as well. Millions were made in the opium trade by businessmen in the Northeast. By 1818, the U.S. was responsible for a third of the opium trade to China. These efforts were justified as "fair, honorable and legitimate trade".
Beginning of Widespread Opium Use in the U.S.
Although opium was available in the U.S., its widespread use did not begin until the Civil War. Opium pills, laudanum (mixture of opium and alcohol), and morphine injections were administered for battle wounds and diarrhea. The Union Army reported to have administered 10 million opium pills with 2.8 million ounces of opium powders and tinctures. Countless veterans became addicted which continued after leaving the army. Addiction was termed "opium slavery" and "morphine mania" and by 1888 Boston reported that 15% of all prescriptions were opiates. Also, during the Civil War, the syringe was invented to administer opium which certainly helped in pain relief but likely increased addiction.
Narcotics in the U.S. were easily available in the late 1800s to 1914. During this time, heroin was briefly sold through Sears & Roebuck catalog for $1.50 and included two vials of heroin, a syringe, two needles and a heroin kit carrying case. This ended with the Harrison Narcotic Act of 1914 with heroin and cocaine as the first two controlled drugs. But "control" was limited to registering with the government and paying a small tax.
Heroin vs. Fentanyl Creation
Heroin is created from opium and was first synthesized in 1874 and promoted by Bayer Company in 1898 as the safer alternative to morphine for pain management and cough suppression. Heroin creation even predates aspirin. Aspirin was also marketed by Bayer, but not available until 1899. To make heroin, the harvested opium latex is dissolved in water, filtered and precipitated with acid to obtain morphine. Morphine is then refluxed with acetic anhydride to create heroin. The process to grow poppies and harvest takes months.
Fentanyl is much easier to create as it can be completed in your garage. The primary starter or "backbone" for the fentanyl molecule is from 4-ANPP and is predominately sourced from a chemical supply business or chemists in China and Southeast Asia. Simple refluxing/mixing of 4-ANPP with propionyl chloride creates fentanyl. One kilogram of 4-ANPP ($800) can make 500,000 pills with a street value of $1 million. Creating your own pills is extremely easy by mixing of the fentanyl powder with compressible sugars and using a $400 pill press purchased online.
Public Availability
Fentanyl is an amazing drug for severe pain relief, but it is also very addictive. The illicit distribution of fentanyl throughout the U.S. as a single drug or mixed with other drugs accounts for at least 70,000 deaths each year. In 2023, the number of these unintentional deaths fell between those attributed to diabetes and kidney disease.
Initially fentanyl was mixed with other narcotics, such as heroin, to create a more potent and addicting narcotic. More than 30 fentanyl derivatives were originally created and distributed as novel compounds which were not under Drug Enforcement Administration (DEA) control. Once the DEA placed all derivatives into Schedule I status, their availability rapidly dropped as the regulatory punishment became the same for distribution of designer or medical fentanyl.
Around the year 2000, the first wave of narcotic abuse in the U.S. started due to opioid prescription overdoses and "fake" pain clinics. The second wave began in 2010 when the DEA countered with a reduction in opioid (oxycodone and hydrocodone) manufacturing, which resulted in a spike in heroin use. The third wave began in 2013 as heroin became in shorter supply and fentanyl became the substitute. But in the current or fourth phase, fentanyl is being mixed with stimulants, such as cocaine and methamphetamine. The combination deaths of fentanyl plus stimulants are nearly identical to fentanyl overdose alone.
CRL Fentanyl Testing Results
CRL has been testing for fentanyl in urine and oral fluids for years. Urine levels have been exceptionally high indicating the drug is routinely ingested and easily detected. The urine median value for fentanyl is 12.6 ng/mL with a high value of more than 36,000 ng/mL. The fentanyl metabolite, norfentanyl, is approximately 4-fold higher than fentanyl.
In oral fluids the levels of fentanyl are reversed with fentanyl levels 5-fold higher than norfentanyl, which also allows for easy detection with a median value of 19.7 ng/mL.
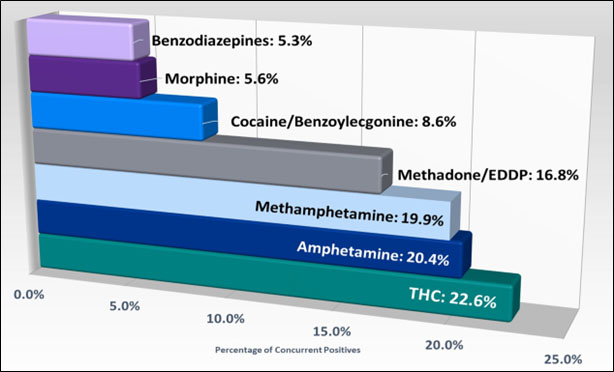
In both urine and oral fluids, the belief that fentanyl is mixed predominantly with other opioids is incorrect based on CRL's retrospective analysis of workplace drug testing results. Only 10% of positive fentanyl samples contain an opioid indicating that other drugs are present. The most common drugs found in a positive fentanyl sample are marijuana, followed by amphetamines, methadone, and cocaine.
The "reasons for test" breakout also provides unexpected findings. The primary reason for drug testing is a pre-employment test. However, 57.5% of all fentanyl positives occur in the random category while pre-employment was only 5.48%. These percentages are nearly the same in oral fluids.
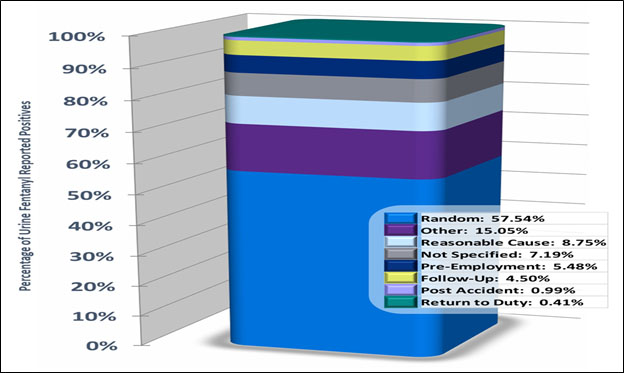
The proposed rationale for the higher rate in random testing is likely the unexpected addition of fentanyl to the company drug testing policy. Pre-employment is likely diminished due to either using a synthetic urine or simply discontinuing all drug use for a few days prior to the test.
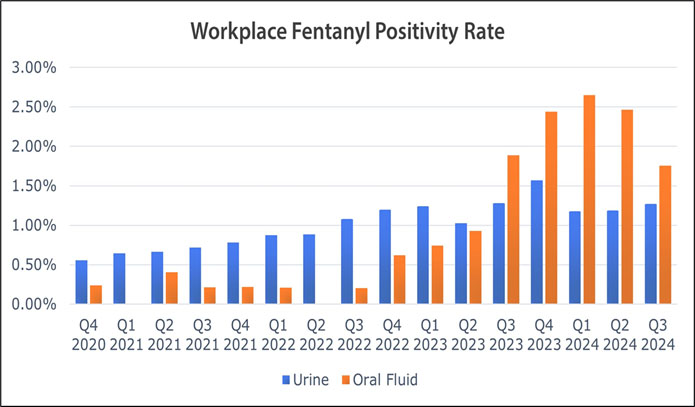
The overall positive percentage of samples tested for fentanyl in urine and oral fluids are dramatic with positive rates in oral fluids substantially higher than urine. In early January 2024, the fentanyl positive rate in oral fluids was greater than 2.5% while urine positivity rate runs between 1-1.5%. This again is likely related to the witnessed oral fluid collection and eliminating synthetic urine substitution.
Summary
The history of the opium trade with China has several similarities to the U.S. war on drugs. In the U.S., drug smuggling is dominated by the Mexican cartels. In the 1700-1800s China had illegal smuggling from Great Britan and the U.S. Due to opium abuse, the Chinese rulers attempted to ban narcotics, just as the U.S. did in the 1980s. China attempted to regulate opium and tax the sale to improve the government financial position. The U.S. is currently trying to regulate and tax marijuana to support schools and roads.
China went through more than a century of drug abuse due to the smuggling of opium into their country by western countries. It now appears the reverse is happening. The basic chemicals for the manufacture of fentanyl are coming from China. Once the popularity of fentanyl is over, the next generation of drugs are already on their shelf and starting to appear in the U.S. Nitazines are 50-fold more potent than fentanyl. Looking for this group of designers will be extremely difficult as fatalities from an even smaller dose are happening.
Fentanyl testing in urine and oral fluids is more important now than ever, as the detection rates are high and continue to increase. The significant impact to safety on the road and workplace cannot be diminished and should be considered part of a drug deterrence program.
Additional Reading
Dalrymple, W., & Cloudlibrary. (2019). The Anarchy: the East India Company, Corporate Violence, and the Pillage of an Empire. S.L.]: Bloomsbury Publishing.
Gerstein, D. R., & Harwood, H. J. (1992). A Century of American Narcotic Policy. Nih.gov; National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK234755/
Goldberg, D. (2009, June 3). Aspirin: Turn-of-the-Century Miracle Drug. Science History Institute. https://www.sciencehistory.org/stories/magazine/aspirin-turn-of-the-century-miracle-drug/
Kadia, M. (2022, March). The Second Opium War: 165 Years Later. Origins. https://origins.osu.edu/read/second-opium-war
Sears Once Sold Heroin. (2019, January 30). The Atlantic. https://www.theatlantic.com/magazine/archive/2019/03/sears-roebuck-bayer-heroin/580441/
Special Reports. (2024, July 25). Fentanyl's deadly chemistry: How criminals make illicit opioids. Reuters. https://www.reuters.com/investigates/special-report/drugs-fentanyl-supply-chain-process/
The American Osteopathic College of Occupational and Preventive Medicine
The American Osteopathic College of Occupational and Preventive Medicine (AOCOPM) stands as a cornerstone organization in advancing occupational and preventive medicine within the medical profession. Since its establishment, AOCOPM has played a pivotal role in shaping workplace health and preventive medicine practices while maintaining the distinctive osteopathic approach to healthcare.
A Legacy of Leadership in Occupational Health
The purpose of the AOCOPM is to promote public health and the practice of preventive medicine with the ultimate goal being to create a better understanding of the relationship of health and prevention in regard to the wellness of the population. The Mission of AOCOPM is to provide education in aerospace, occupational, environmental, and preventive medicine and to encourage member activity and leadership within the College and other prevention-oriented healthcare organizations. The organization serves as both a professional home for physicians specializing in aerospace, occupational medicine and preventive medicine, and as a driving force for advancing these specialized fields within the broader medical community.
Educational Excellence and Professional Development
At the heart of AOCOPM's activities lies a robust commitment to education and professional development. The organization provides comprehensive continuing medical education programs that blend traditional occupational medicine principles with osteopathic philosophy. Their educational initiatives include:
- AOCOPM maintains a significant presence at the American Osteopathic Association's annual OMED conference, where they offer specialized tracks in aerospace, occupational and preventive medicine. These sessions provide members with valuable opportunities to earn CME credits while engaging with cutting-edge developments in the field. The organization's participation in OMED also facilitates cross-specialty collaboration and helps integrate occupational and preventive medicine perspectives into broader osteopathic practice. We have partnered with organizations, such as the AOA's Bureau of Public Health, the Association of Military Osteopathic Physicians and Surgeons, and the American College of Osteopathic Family Physicians to provide conjoined lectures.
- The AOCOPM Midyear Educational Conference brings together leading experts and practitioners to share latest developments and best practices in the field. This flagship event serves as a crucial platform for knowledge exchange and professional networking.
- The commemorative lecture series features distinguished speakers who have made significant contributions to occupational and preventive medicine. These lectures honor pioneering figures in the field while providing current practitioners with insights into emerging trends and challenges. The organization has also developed courses and partnerships to physicians seeking continuing medical education and credentials in corrective/carceral medicine, undersea hyperbaric medicine, and disability impairment medicine.
Distinctive Osteopathic Approach
What sets AOCOPM apart is its integration of osteopathic principles into occupational and preventive medicine. This unique approach emphasizes:
- Holistic evaluation of workplace health issues, considering the interconnectedness of body systems and environmental factors
- Preventive strategies that address both individual and workplace-wide health concerns
- Implementation of osteopathic manipulative treatment (OMT) when appropriate in occupational medicine settings
- Recognition of the body's inherent ability to heal and maintain health, informing both treatment and prevention strategies
Leadership and Governance
AOCOPM's effectiveness stems from its strong leadership structure. The organization is guided by a board of trustees comprising experienced practitioners who bring diverse expertise to their roles. These leaders work to ensure that AOCOPM remains at the forefront of occupational and preventive medicine while upholding osteopathic principles and practice.
The leadership team focuses on:
- Setting strategic direction for the organization
- Developing and implementing educational programs
- Advocating for the profession at national and state levels
- Fostering relationships with other medical organizations and stakeholder groups
Impact on Workplace Health
AOCOPM's influence extends beyond its immediate membership to impact workplace health practices across the United States. The organization's members serve in various capacities:
- As corporate medical directors shaping company-wide health policies
- In government agencies developing occupational health regulations
- As independent consultants advising on workplace safety and health programs
- In academic institutions training the next generation of occupational medicine specialists
Advocacy and Professional Recognition
AOCOPM serves as a strong advocate for occupational and preventive medicine within the osteopathic profession and broader medical community. The organization works to:
- Enhance recognition of osteopathic occupational medicine specialists
- Influence policy decisions affecting workplace health and safety via non-lobbying educational efforts
- Promote evidence-based practices in occupational and preventive medicine
- Support members in their professional development and career advancement
Future Direction and Challenges
As workplace environments evolve and new occupational health challenges emerge, AOCOPM continues to adapt and lead. The organization focuses on addressing contemporary issues such as:
- The impact of technological change on workplace health
- Environmental health concerns in occupational settings
- Mental health and wellness in the workplace
- Integration of preventive medicine principles in occupational health programs
- Engaging the next generation of medical students and residents
Member Services and Support
AOCOPM provides comprehensive support to its members through:
- Access to specialized continuing medical education programs
- Networking opportunities with fellow practitioners
- Resources for practice management and professional development
- Updates on regulatory changes and industry developments
- Scholarships for first-time osteopathic board certification
Community Engagement and Partnerships
The organization maintains strong relationships with:
- Other osteopathic specialty colleges
- Occupational health organizations
- Governmental agencies
- Corporate health departments
- Academic institutions
These partnerships enable AOCOPM to expand its influence and better serve its members while advancing the field of occupational and preventive medicine.
Conclusion
AOCOPM continues to play a vital role in advancing workplace health and preventive medicine practices. Through its commitment to education, AOCOPM ensures that osteopathic physicians remain at the forefront of occupational and preventive medicine, bringing their unique perspective and skills to workplace health challenges across the nation.
The organization's diverse membership base includes subject matter experts throughout government, education and industry. This network of quality physicians willingly shares best practices and collegial support and brings a distinctive approach to workplace health that benefits both practitioners and patients. As workplace health challenges continue to evolve, AOCOPM's leadership and guidance will remain essential in shaping the future of aerospace, occupational and preventive medicine within the medical profession.
MRO Semiannual Reporting Requirement
(July-December 2024)
The October 12, 2023, Mandatory Guidelines for Federal Workplace Drug Testing Programs using Urine (UrMG) (effective February 1, 2024) and Mandatory Guidelines for Federal Workplace Drug Testing Programs using Oral Fluid (OFMG) (effective October 10, 2023) added a requirement for MROs to submit semiannual reports to the Secretary, or designated HHS representative, on federal agency specimens that were reported as positive for a drug or drug metabolite by a laboratory and verified as negative by the MRO. The report must not include any personally identifiable information for the donor and must be submitted within 14 working days after the end of the semiannual period (i.e., in January and July).
Please refer to UrMG and OFMG Section 13.11 for more detail.
All MROs that work with federal agency specimens should register with the National Laboratory Certification Program (NLCP) to begin submitting semiannual reports.
MROs who have already registered with the NLCP should have received an email with instructions for submitting your July - December 2024 MRO Semiannual Report. If you did not receive this email, please register again via the link below.
MROs who have not registered with the NLCP should click the link below to register and submit your July - December 2024 MRO Semiannual Report no later than January 22, 2025.
Register HereOnce registered, you should receive a confirmation email including your MRO ID and instructions on how to submit the semiannual report. Please share your MRO ID with any other registered MROs that will be submitting reports on your behalf.
Please send an email to mbrogdon@rti.org if there are issues, or you don't receive a confirmation email.
Please contact the NLCP staff at nlcp@rti.org if you have any questions concerning this notice.
Useful Documents
NLCP MRO Semiannual Reporting template (Excel)
MRO Reporting Requirement Instructions (PDF)
ODAPC - DOT
- Office of Drug & Alcohol Policy & Compliance (ODAPC)
- DOT 49 CFR Part 40 Procedures for Transportation Workplace Drug and Alcohol Testing Programs
- Subscribe to the ODAPC Updates and News
- 2024 DOT Random Testing Rates
SAMHSA - HHS
- Medical Review Officer Guidance Manual for Federal Workplace Drug Testing Programs
- Mandatory Guidelines for Federal Workplace Drug Testing Programs using Urine (UrMG)
- Mandatory Guidelines for Federal Workplace Drug Testing Programs using Oral Fluid (OFMG)
NRC
CUSTODY AND CONTROL FORMS (CCFs)
- 2020 Federal CCF for Urine and Oral Fluid Specimens
- 2020 Guidance for Using the Federal CCF for Urine Specimens


Medical Review Officer
Certification Council (MROCC)
3231 S Halsted St, Ste Front #167
Chicago, IL 60608
Tel: 847.631.0599
Email: mrocc@mrocc.org
Co-editor: James Ferguson, DO
Co-editor: Donna Smith, PhD
Managing Editor: Kristine Pasciak
©2024 Medical Review Officer Certification Council
ISSN: 2833-0870
MRO Quarterly is an educational publication intended to provide information and opinion to health professionals. The statements and opinions contained in this document are solely those of the individual authors/contributors and not MROCC. MROCC and its editorial staff disclaim responsibility for any injury to persons or property resulting from any ideas or products referred to in this newsletter.
To unsubscribe from MROCC emails, please send an email to mrocc@mrocc.org with the subject unsubscribe.
